What Medicare Covers for Home Dialysis

Medicare is a complex program, and it is easy to become confused about or misunderstand it. I can’t count the number of times patients and staff have shared incorrect information about Medicare coverage for home dialysis. I decided to write this blog to try to set the record straight. My hope is that the information I provide here will help staff to explain to patients and patients to advocate with dialysis providers for what they need when Medicare covers it.
Who Can Get Medicare
People are eligible for Medicare at age 65 or when they have received Social Security Disability Insurance checks for 24 months.
People with end-stage renal disease (ESRD, or permanent kidney failure) can apply for Medicare if they are in the U.S. legally and have enough work credits as a worker, spouse, or child of a worker. Medicare based on ESRD can start the 1st month of dialysis IF they start PD or HD home training before the end of the 3rd month of dialysis. Otherwise, they have to wait 3 months for Medicare to start if they begin home training later.
People with acute kidney injury (AKI) are not eligible for Medicare due to ESRD—but can be eligible for Medicare due to age or disability.

How Medicare Pays for Dialysis
Medicare pays a flat (bundled) rate for dialysis under the ESRD prospective payment system (PPS). Medicare’s payment for in-center and home dialysis treatments is the same. In the ESRD PPS 2025 proposed rule, the Centers for Medicare and Medicaid Services (CMS) proposes a base payment for dialysis of $273.20 with clinic- and patient-level adjustments. There are add-on payments for new and innovative devices as well. The Medicare PPS covers ESRD-related blood tests and medications, too. Unless lobbying stops it, starting in 2025, oral phosphate binders will be added to the ESRD PPS. A fact sheet describes proposed changes.
How Medicare Pays for Home Dialysis Training
When someone starts dialysis, Medicare pays the clinic the ESRD PPS plus an onset of dialysis adjustment that raises payment for the first 120 days. Starting in 2016, the add-on was 32.7%.
In the first 120 days when clinics get the add-on, Medicare won’t pay clinics more for home dialysis training.
After those 120 days, Medicare will pay clinics a training adjustment add-on fee for each training day.
In the proposed rule, CMS proposes a training add-on fee of $95.57 per training day for PD or home HD in 2025.
Medicare covers up to 15 PD training sessions and up to 25 home HD training sessions. CMS is proposing in 2025 to start covering training for Medicare patients with AKI.
What Medicare Expects Clinics to Provide to Home Dialysis Patients with Medicare
I’m sure everyone knows that under the ESRD PPS, Medicare expects dialysis clinics to provide all the HD and PD equipment and supplies required to do dialysis. But, did you know that the Medicare Benefit Policy Manual, Chapter 11 End Stage Renal Disease (ESRD) states this? (Bold emphasis is mine).
20.4 - Equipment and Supplies
(Rev. 200, Issued: 12-02-14, Effective: 01-01-15, Implementation: 01-05-15)
All medically necessary equipment and supplies used to furnish dialysis (in-facility or in a patient’s home) are included in the ESRD PPS and are not separately paid as of January 1, 2011. The equipment and supplies include but are not limited to
Equipment and supplies included under the composite rate (see §20.1 of this chapter) as of December 31, 2010,
Equipment and supplies that were billed by ESRD facilities and paid separately by Medicare, and
Equipment and supplies furnished to home patients that were under Method II prior to January 1, 2011, and billed by Durable Medical Equipment (DME) suppliers and paid separately by Medicare.
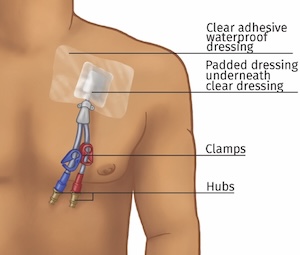
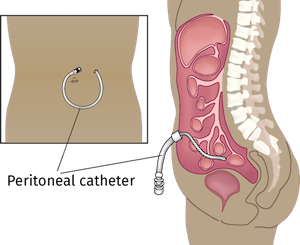
ESRD facilities and monthly capitation payment practitioners may determine that it is medically necessary for a dialysis patient to use dressings or protective access coverings, including catheter coverings, on their access site. All medically necessary dressings or protective access coverings used during or after dialysis to protect a dialysis patient’s access site including for example, coverings used for day-to-day activities such as bathing, are considered to be renal dialysis items. To the extent that dressings and protective access coverings, including catheter coverings, are determined to be medically necessary, an ESRD facility should provide them. Medicare payment for vascular access equipment and supplies is included in the ESRD PPS for all dialysis patients regardless of the method of dialysis or where they receive dialysis treatments.
Separate payment for renal dialysis equipment and supplies is not made under the ESRD PPS or under the blended payment during the ESRD PPS transition.
ESRD facilities may not receive payment for renal dialysis equipment and supplies from ESRD beneficiaries.
Home Dialysis Equipment and Supplies
All home dialysis equipment, supplies, and other medically necessary items for home dialysis ordered by a physician were included in the composite rate and are therefore included under the ESRD PPS. The ESRD facility with which the patient is associated assumes responsibility for providing all home dialysis equipment, supplies, and support services either directly or under arrangements to all of its home dialysis patients.
Home Dialysis Equipment Provided to Home Hemodialysis and Peritoneal Dialysis Patients Coverage of any item of home dialysis equipment used for home dialysis depends on its medical necessity. Medical necessity is established by the physician’s order, and by the equipment meeting Medicare guidelines that define home dialysis equipment.
Nonmedical items are also included in the ESRD PPS and may not be billed separately. For example, if a home patient is wheelchair bound and it is medically necessary for the patient to weigh themselves before and after a dialysis treatment, the ESRD facility is responsible for furnishing the patient with a wheelchair scale.
Installation and Delivery of Home Dialysis Equipment

ESRD facilities are responsible for all reasonable and necessary expenses incurred in the original installation of home dialysis equipment. This coverage is not extended to expenses attributable to home improvement (e.g., plumbing or electrical work beyond that necessary to tie in with existing plumbing and power lines). Testing and assurance of equipment performance, which may be billed for as part of the basic delivery charge, are also covered. Medicare does not cover maintenance contracts on equipment, since Medicare pays only for costs that are actually incurred. The delivery and installation charge should be itemized, either on the face of the bill or an attached invoice.
Other Requirements for Coverage of Home Dialysis Equipment

Supportive equipment that is used in conjunction with the basic dialysate delivery system. This includes blood, heparin pumps, air bubble detectors, blood leak detectors, and unipuncture devices.
Adjustable chairs, such as recliners, as these chairs serve to preserve patients’ health by allowing rapid manipulation in body position when medical circumstances warrant such changes during dialysis (e.g., when acute hypotension occurs and the patient is in danger of going into shock).
Effective for renal dialysis services provided on or after January 1, 2011, the ESRD facility is responsible for fulfilling the requirements necessary for furnishing home dialysis. This includes but is not limited to:
Home dialysis equipment must also meet the requirements outlined in Pub. 100-02, Medicare Benefit Policy Manual, chapter 15, §110.
Home Dialysis Supplies Provided to Home Hemodialysis and Peritoneal Dialysis Patients
ESRD facilities are responsible for supplies necessary for the effective performance of all modalities of home dialysis, for example, alcohol wipes, sterile drapes, gloves, telfa pads, bandages, etc. Necessary supplies could also include but are not limited to start-up durable supplies (whether or not they are part of a start-up kit) such as weight scales, sphygmomanometer, I.V. stand, and dialysate heaters; and consumable and disposable supplies such as dialysate, tubing, and gauze pads.
Instruments and nonmedical supplies, such as scales, stopwatches, and blood pressure apparatus (this does not include automatic blood pressure monitoring devices such as those mentioned in Pub. 100-03, Medicare National Coverage Determinations Manual, Chapter 3), are included in the ESRD PPS, regardless of whether provided separately or as part of a start-up kit.
Coverage for Surgical Dressings
When dialysis access has been surgically placed in a patient to enable an ESRD facility to provide dialysis treatment, and the patient has started dialysis, the dressing changes are part of the home support provided by the ESRD facility. When surgical wounds are not related to ESRD, the patient may be eligible for care under the home health benefit found in §20.4.C of this chapter.
The CMS webpage on ESRD PPS Consolidated Billing for CY 2024 also lists as covered home dialysis supplies and equipment:
IV stand
Topical and injectable anesthetics
Electric heating pad for PD
PD anchoring device or belt
Thermometer, reusable oral
In addition, the ESRD PPS Consolidated Billing List includes a list of ESRD-related labs and ESRD-related medications in these categories:
Access management
Anemia management
Bone and mineral metabolism
Cellular management
Anti-infectives
Composite rate (old payment system) drugs
I have always wondered if a dialysis clinic would be required to provide a bed scale or Hoyer lifts for a bedbound patient, so I emailed ESRDPayment@cms.hhs.gov. This is the response I received: “We would encourage an ESRD facility to consider the medical necessity for alternative methods of weighing beneficiaries who are bedbound. Medical necessity can be established by the physician’s order, and by the equipment meeting Medicare guidelines that define home dialysis equipment. Please see Medicare Benefit Policy Manual in section 20.4.A.1.” That is the shaded text above. That text also refers to Pub. 100-02, Medicare Benefit Policy Manual, chapter 15, §110, which is the manual where CMS defines durable medical equipment.
Conclusion
It’s important for dialysis management and staff to be aware of what Medicare requires clinics to provide under the reimbursement they receive for Medicare patients with ESRD and AKI. No provider should ever tell a patient that items or services described in the Medicare Benefit Policy Manual for ESRD or listed in ESRD PPS Consolidated Billing are the patient’s responsibility. No one wants their dialysis clinic accused of fraud & abuse.


Comments
Beth Witten
Sep 13, 2024 2:55 PM
Tyrone Davis
Sep 13, 2024 11:08 AM